Common GI Conditions
-
Celiac Disease
-
Hepatitis A,B & C
-
IBS - Irritable Bowel Syndrome
-
Crohn's and Colitis
-
Peptic Ulcer Disease
-
Hemorrhoids
-
Gallstones
-
Colon Polyps and Colon Cancer
-
Barrett's Esophagus
-
Gastroesophageal Reflux Disease (G.E.R.D.)
Celiac Disease
Celiac Disease is an allergy to gliadin, a protein component of gluten, which is found in wheat and other grains. It was originally thought to be a relatively rare disease, primarily of childhood, and in adults presenting with severe diarrhea, weight loss and malnutrition. We now know it to be far more common than previously thought, and is present in 1.3 and 3 million Americans. The symptoms also are not necessarily as obvious as once thought. Although diarrhea is still the most common symptom, patients may present with iron deficiency anemia, abdominal pain, unexplained weight loss or abnormal liver function tests. Celiac disease can be diagnosed with a screening blood test, but biopsy of the small intestine (a simple out-patient procedure) is recommended to confirm the diagnosis. A trial of a Gluten-free diet is not recommended before a firm diagnosis is made, as that diet is very restrictive and expensive, and the response may be subjective. Only when the diagnosis is sure should patients be placed on this difficult diet.
Hepatitis A,B & C
There are three major viruses that cause viral hepatitis (inflammation of the liver): A, B and C. Hepatitis A is what was referred to as infectious hepatitis many years ago. It is spread by the fecal-oral route, meaning it is ingested in foods that have been contaminated by stool containing the virus, oysters being a common culprit. Patients are contagious early in the disease before they turn yellow. It is mostly a disease of childhood and many adults are immune without knowing they ever had it. It is generally a benign disease in children, but can be more severe and even occasionally fatal in adults. The major symptoms are jaundice (yellow eyes), fatigue and anorexia. There are blood tests to diagnose the acute illness and to check for prior immunity. The disease never goes on to any chronic form. There is no specific treatment once the virus has taken hold, but an effective vaccine exists. The vaccine is recommended for adults who have other liver problems and could not handle another insult to the liver and to people traveling to South America or Asia.
Hepatitis B, the old "serum hepatitis," is spread mostly through contact with blood or other body fluids. It can, therefore, be spread sexually or during childbirth, as well as through needle sticks or intravenous drugs. Donated blood is carefully screened for hepatitis B, so transmission that way is now extremely rare. The initial symptoms are quite similar to A, but unlike A, about 5% of patients develop a chronic form of the disease, either a chronic carrier state or ongoing damage to liver. Long term infection with B may lead to cirrhosis or cancer of the liver. There are several treatments available for chronic hepatitis B, but more importantly an excellent vaccine exists and it is recommended all children be vaccinated before starting college.
Hepatitis C represents the greatest problem in the Unites States. Unlike the others, the initial infection is often asymptomatic, but 85% of patients go on to develop a chronic form of the disease. They often present later in life when routine blood tests show abnormal liver function. Specific blood tests then can assist the physician in diagnosing the type of virus and the amount in the bloodstream. Many patients contracted C from intravenous drug use, often many years in the past, or from blood transfusions years ago. Currently, all donated blood used is carefully screened (as for B) so this form is no longer likely. There are estimated to be 3 million people in the U.S. with C, and many will go on to develop cirrhosis or liver cancer, if not treated. A fairly effective, though difficult, treatment exists, and this can be explained to you by an AIG doctor, all of whom have extensive experience with this disorder. There is, unfortunately, no vaccine for C.
IBS - Irritable Bowel Syndrome
Irritable Bowel Syndrome (IBS) is a condition in which there is a disturbance in the function of the gastrointestinal tract. Patients may complain of abdominal pain, bloating, or a change in bowel habits (diarrhea, constipation, or alternating diarrhea and constipation). In contrast to Inflammatory Bowel Disease (IBD), patients do not have more severe issues such as weight loss, fever, bleeding, and anemia. Irritable Bowel Syndrome affects one in five Americans and is more common in women. The syndrome usually begins in late adolescence and does not typically begin for the first time after age 50.
The exact cause of IBS is not known, but experts believe it is related to an increased hypersensitivity or stimulation of nerves of the gastrointestinal tract. Many patients find that their IBS is triggered by emotional stress as well as oral intake. Greasy or spicy foods or diary products can irritate the intestines. Beverages that contain alcohol or caffeine can also aggravate symptoms.
Irritable Bowel Syndrome is a functional disorder. There is no underlying anatomical abnormality. Although IBS is uncomfortable and inconvenient, it is not life threatening. To diagnose IBS, your doctor will want to rule out more serious conditions. This process may entail blood tests, X-rays, and/or endoscopy.
The treatment of IBS is based on the patient’s particular symptoms. Keeping a diary of symptoms will help guide the specific regimen. Often increasing the amount of fiber and fluids in addition to avoiding triggers in your diet can relieve symptoms. If necessary, fiber supplements or anti-spasmotic medications can be used. The key to successful treatment of IBS is to establish and maintain a good treatment plan with your gastroenterologis.
Crohn's and Colitis
The term Inflammatory Bowel Disease (IBD) represents two diseases: ulcerative colitis and Crohn’s disease. Both conditions involve inflammation of the gastrointestinal tract that can cause weight loss, abdominal pain, bleeding and diarrhea. Frequently, IBD presents during adolescence, but people of any age can be afflicted. The exact cause of IBD is not known, but there are definite genetic and environmental factors.
In ulcerative colitis (UC), inflammation is limited to the colon and rectum. Patients often complain of diarrhea and passing blood and mucus in their stool. UC is diagnosed with a colonoscopy.
Treatment for ulcerative colitis includes medications given by mouth or by suppository/enema to control the inflammation. For more aggressive disease, treatment involves the use of steroids that are given by mouth or intravenously while in the hospital.
In contrast to ulcerative colitis, Crohn’s disease can affect any part of the gastrointestinal tract, mouth to anus. Patients may complain of abdominal pain, nausea, vomiting, diarrhea and weight loss. In order to diagnose Crohn’s disease (and distinguish between ulcerative colitis or even irritable bowel syndrome (IBS)), patients may require blood tests, colonoscopy, and/or barium X-rays.
Similar to ulcerative colitis, treatment of Crohn’s disease consists of anti-inflammatory medications, sometimes including steroids or other agents. In cases that fail to respond to medications, occasionally surgery is necessary.
Peptic Ulcer Disease
Peptic Ulcer Disease is a common cause of abdominal pain and gastrointestinal bleeding. Patients may present with burning epigastric discomfort (that may improve with food), black stool, vomiting blood or very dark material or simply iron deficiency anemia. After evaluation by a gastroenterologist, an upper endoscopy may be performed to make the diagnosis. Under sedation, a flexible endoscope is passed through the mouth and the esophagus, stomach and first portion of the small intestine or duodenum, which are examined carefully.
The vast majority of ulcers are caused by a bacteria known as Helicobacter pylori, which can be found in at least 50% of patients over the age of 60 in the United States. The gold standard for diagnosing H. pylori is by taking a biopsy at the time of endoscopy, although less sensitive and specific blood and breath tests are available. The use of aspirin and NSAIDs (non-steroidal anti-inflammatory drugs such as ibuprofen and naprosyn) are the other most common causes of ulcers. An extremely small proportion of gastric ulcers are malignant. Treatment of peptic ulcer disease includes acid suppression (typically with a class of medications known as proton pump inhibitors), eradication of H. pylori, if present, (with a two week course of antibiotics) and discontinuation of NSAIDs, if medically possible. Severe gastrointestinal bleeding may be controlled at the time of endoscopy with electrocautery or injections of medication. Your physician can discuss other details regarding diagnosis, treatment and the appropriate follow-up with you in the office.
Hemorrhoids
Hemorrhoids are swollen blood vessels in the anal region. The blood vessels usually become swollen by straining during bowel movements. Hemorrhoids can develop both inside and outside the rectum and are usually painful, accompanied with some bleeding. Other symptoms of hemorrhoids include itching and a change of the stool shape or caliber.
Hemorrhoids are more common in women (particularly after pregnancy) and usually after the age of 30. They are commonly seen in people who are constipated, but also can occur in people without any bowel problems.
Treatment of hemorrhoids includes sitz bath (warm bath for more than 20 minutes), topical ointments and creams and regulating bowel movements. High fiber diets, increasing fluid intake, fiber supplements and stool softeners can correct constipation and straining. Twenty to thirty grams of fiber are recommended daily. Chronically painful or bleeding hemorrhoids may need to be treated with banding or surgery. Consult your physician with questions or problems.
Gallstones
Gallstone disease is one of the most common of all digestive diseases. Ultrasound provides a rapid and risk free method to diagnose gallstones. For the majority of patients, gallstones are found incidentally when radiographic imaging is performed for another reason. Twenty percent of patients with incidental gallstones will develop symptoms over the next fifteen years. Overall, approximately ten percent of the population have gallstones, which is more prevalent in females and older age groups. People who develop symptoms are likely to develop recurrent symptoms. Symptoms are referred to as biliary colic – moderately severe right upper quadrant pain radiating to the back and right shoulder with associated nausea. Symptomatic disease is seen more frequently in diabetics, gastric bypass patients, patients with rapid weight loss and pregnant women. Patients with symptoms should seek medical attention.
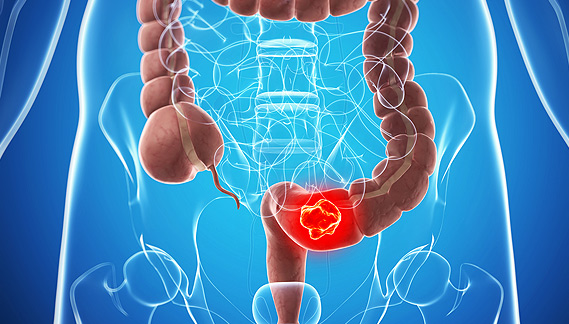
Colon Polyps and Colon Cancer
Colon cancer is the second leading cause of cancer death in the United States and affects men and women equally. However, colon cancer is one of the most preventable and curable forms of cancer. Colon cancers almost always begin with polyps. Polyps are small growths of fleshy tumors that occur on the inside lining of the colon. Colon polyps start out as benign tumors and are very slow growing. However, over the course of years, as they enlarge, the risk of cancer increases. Colon cancer can be prevented by removing polyps during a colonoscopy.
There are certain risk factors for the development of colon cancer, which include: age over 50, a family history of colon cancer or polyps, polyposis syndromes and inflammatory bowel disease (Crohn’s disease and ulcerative colitis). Other possible risk factors include obesity, significant alcohol use, smoking, diabetes, physical inactivity and a diet high in animal sources (low in fiber).
The best way to prevent colon cancer is to screen for it and remove polyps before they become cancerous. Screening tools include: stool tests to detect occult (hidden) blood, sigmoidoscopy, barium enema and colonoscopy. Colonoscopy is the “Gold Standard” for prevention, detection and removal of polyps and colon cancer.
Anyone over the age of 50 should be screened and those with risk factors should begin screening in their 30’s or 40’s. Colon cancer is preventable. Ask you doctor what is appropriate for you today.
Barrett's Esophagus
Barrett’s esophagus is a condition in which the lining of the esophagus (swallowing tube) changes, becoming similar to the tissue that lines the intestine. Barrett’s is a complication of gastroesophageal reflux disease (GERD) and is more likely to occur in patients who either experienced GERD at a young age or have a longer duration of symptoms. Barrett’s esophagus is diagnosed at the time of an upper endoscopy and confirmed by biopsies taken during the endoscopy. There is a small but not insignificant risk of developing esophageal cancer in patients with Barrett’s esophagus (approximately 0.5 percent per year). Dysplasia, which is discovered via biopsy obtained during endoscopy, is a precancerous condition in patients with long term Barrett’s and may progress to esophageal cancer.Therefore, patients with Barrett’s should be screened every 2 – 3 years with endoscopies to prevent the progression to esophageal cancer. Those with dysplasia are monitored more closely. There is no cure for Barrett’s, although it has been suggested that treating GERD symptoms with medication may prevent the progression of the disease.
Gastroesophageal Reflux Disease (G.E.R.D.)
GERD (gastro-esophageal reflux disease) is a common condition affecting approximately 20 million Americans. It is caused by inappropriate relaxations of the muscle between the stomach and esophagus (lower esophageal sphincter), which allows stomach acid to come up into the esophagus. GERD may be either erosive (causing esophagitis or damage to the lining of the esophagus) or non-erosive. The major symptom of GERD is heartburn. Almost everyone may have occasional heartburn, but when it occurs more than twice a week, causes nocturnal awakening or is associated with difficulty swallowing or bleeding, medical attention is necessary. There are also so-called extra-esophageal symptoms of GERD including cough, hoarseness, sore throat, asthma or chest pain. All these symptoms may have other causes and proper diagnosis is important. The physicians of Affiliates in Gastroenterology are all skilled in the latest modalities in the diagnosis and treatment of GERD.
